IBS is a common digestive complaint affecting between 1/10 and 1/5 of the population. As yet, there is no agreed upon consensus to explain why it develops, although some people can find patterns to explain why their symptoms flare up when they do.
What are the Symptoms of IBS?
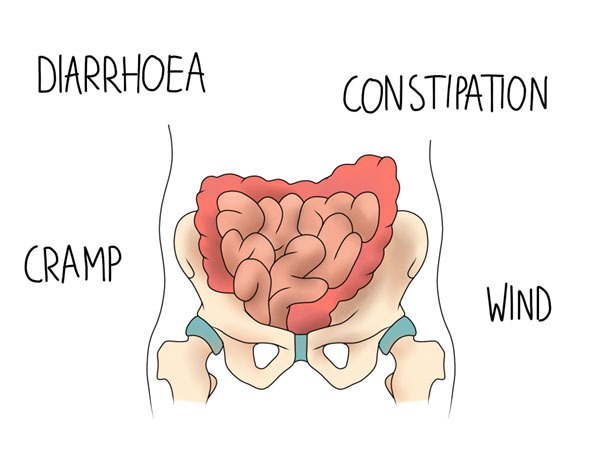
There are a range of symptoms associated with the condition. They are variable between people, and for an individual, with swings from diarrhoea to constipation being common. They include:
- cramping
- wind
- bloating
- diarrhoea
- constipation
Abdominal pain can be associated with a number of these symptoms, and again, is likely to fluctuate.
Causes and Triggers
Frustratingly, the root causes for IBS are unknown. Theoretical mechanisms to explain the condition are difficult to prove, but patients often report links to stress and diet. A theory to explain this is that in IBS, the gut fluctuates between higher and lower motility than usual. Stress, and the fight or flight response area easily linked here. High caffeine intake has been linked to IBS, as have FODMAP sugars, which is an abbreviation for
Fermentable
Oligosaccharides,
Disaccharides,
Monosaccharides, and
Polyols.
Up to 75% of people with IBS may find an improvement in symptoms when they reduce their FODMAPs. This makes sense as these sugars can contribute to gassiness due to their fermentability, therefore leading to bloating and cramping. But because these sugars are so widespread in whole foods, including fruit, vegetables, milk, and grains, they can be hard to identify without more thorough investigation.
Differences with IBD
IBD stands for inflammatory bowel disease. This is an umbrella term for ulcerative colitis and Crohn’s disease. Both of these conditions are autoimmune, and may have a genetic link. They can also be associated with rheumatological conditions that affect the joints, such as ankylosing spondylitis (AS) and rheumatoid arthritis (RA). It can be useful for your osteopath to know about a personal or family history of IBD as a result.
The similarities between IBS and IBD are a good reason for thorough investigation before diagnosing either condition. IBS is not a diagnosis that should be given to you in the absence of investigations to rule out other problems. IBS should be considered by your GP when you have at least 6 months of any or all of the following:
A: abdominal discomfort
B: bloating
C: changes to bowel habits
If further indicators remain for IBS, the NHS recommends a blood test to screen for other conditions.
Managing IBS
Understanding your triggers may be the easiest way to manage your IBS and limit flare ups in the long term. Keeping a diary to log your symptoms, diet, and stress might help you identify the triggers. Hormonal changes may also be relevant, especially if you are peri-menopausal or have any endocrine issues.
A study based on traditional Chinese joint manipulation techniques found that symptoms of IBS may be improved by clicking the joints in the lower back. The study was relatively large, involving 200 participants, and it compared the results of joint manipulation against medication. Results were statistically significant, with those undergoing manipulation experiencing a significant reduction in pain, as well as the frequency and severity of symptoms. The researchers’ explanation for this was that “displaced” discs could be causing a problem with the nerves that could lead to IBS. However we know that manipulation does not pop discs back in (nor do discs become displaced, they are firmly connected above and below), but there may still be some merit to the research.
Some osteopaths use more direct techniques to address abdominal problems. These are known as “visceral techniques”, and include work to the organs within the abdomen with the aim of releasing tension and improving function. Some people find that this approach helps them to manage their symptoms.
Potential Effects of IBS on the Musculoskeletal System
We can also theorise that the abdominal pain of IBS could cause a change in posture. Acute abdominal pain often causes us to subconsciously hunch over into a more protected position. However, we know that maintaining this position for long periods (such as working at a desk) can lead to some musculoskeletal issues. Typically these include:
- upper back tension (which may be asymptomatic)
- headaches
- lower back pain
- tight chest muscles and rounded shoulders
A lot of these symptoms can be linked back to the upper back tension, and often treatment will involve work to improve movement in the upper back. Upper back stiffness places more demand on the areas above and below it, leading to the potential for neck and lower back pain. Keeping that upper back stiffness at bay may prevent the secondary aches and pains elsewhere.
Make an osteopathy appointment in Leeds here
References
- Nice.org.uk. 2022. Introduction | Irritable bowel syndrome in adults: diagnosis and management | Guidance | NICE. [online] Available at: <https://www.nice.org.uk/guidance/cg61/chapter/introduction> [Accessed 3 August 2022].
- The IBS Network. 2022. FODMAPS: What are FODMAPS?. [online] Available at: <https://www.theibsnetwork.org/diet/fodmaps/> [Accessed 26 July 2022].
- Qu, L., Xing, L., Norman, W., Chen, H. and Gao, S., 2012. Irritable bowel syndrome treated by traditional Chinese spinal orthopedic manipulation. Journal of Traditional Chinese Medicine, 32(4), pp.565-570.
- Snelling, N., 2006. Do any treatments work for irritable bowel syndrome?. International Journal of Osteopathic Medicine, 9(4), pp.137-142.