Reflux is a common problem for adults and infants alike. Studies show that over 25% of babies experience reflux symptoms in the first year of life. Western cultures see roughly 20% of adults affected too. Although symptoms present differently in adults and babies, the mechanism is the same: stomach acid flows back up to the oesophagus (food pipe) causing chest pain and sometimes vomiting.
Infant Reflux
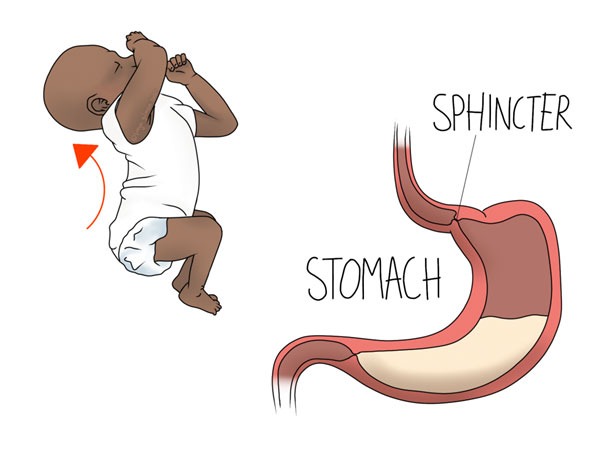
A combination of a liquid diet, lots of time laying down, and developing musculature form the perfect storm in which infant reflux can develop.
Although this condition is very common and usually self limiting (most cases resolve by baby’s first birthday), it can cause a lot of anxiety for parents. Spit-up is generally no cause for concern, but frequently regurgitating after feeds can make it look like baby is not getting as much nutrition as they need. If you are concerned, contact your GP or health visitor, and you might find it useful to spill a teaspoon or tablespoon of milk or yogurt on fabric to see how far it spreads. It’s often surprising how far it goes, making a small spit up look much more significant. However, if you are concerned about baby’s weight gain slowing down, or a reduction in nappy output, seek medical attention.
Signs and Symptoms of Infant Reflux
Timing is key, as reflux is much more likely to occur within a few minutes of feeding. Babies who are especially fussy after eating (especially when laid down after a meal), may be trying to express their discomfort. The hallmark sign of upset due to reflux is the arched-back position illustrated above. Baby stretches out their tummy to try and find relief, and may bring their legs up higher.
Colic is a collection of symptoms affecting young babies, including extended periods of crying. There is no single cause for it, but digestive issues like this are often cited as a possibility. Read more about colic here.
Silent Reflux
Even if your baby does not spit up, they may still be suffering with reflux. If the other symptoms of discomfort are present, especially if they closely follow feeds, they may have silent reflux.
Managing Infant Reflux
Infant reflux usually resolves on its own in time, but there are changes you can make in the meantime to negate the symptoms. Even if your baby is too young to sit unaided, it’s safe for them to sit supported for short periods. Sitting them on your lap or in a relatively upright baby seat after eating can give the stomach a chance to empty a bit before laying them down. Winding after a feed to ensure the stomach is no more full than it should be might also help.
Although the liquid diet likely contributes to the symptoms, put safety first. Do not be tempted to introduce solids early (before 6 months) without the support of your baby’s doctor. In a similar vein, do not sacrifice safe sleep in an attempt to ease symptoms. Although a lot of cots are sold with “anti-reflux” features such as mattresses with adjustable angles, these may not be safe. For safe sleep, babies should be put down on their backs, on a firm, flat surface. Again, it is up to your doctor to make an exception based on your baby’s specific case.
Our paediatric osteopaths may be able to help your baby find comfort with gentle techniques for the head and abdomen.
Adult Reflux or Heartburn
The mechanism is much the same in adult heartburn as above, although some of the factors are different. A liquid diet may play a role for infants, but some solid foods may make your adult reflux worse. Keeping a food and symptom diary may be useful here. Other risk factors include:
Possible Factors
- Pregnancy
- Overeating
- Eating soon before bed or before laying down
- Some medicines
There may also be a link with alcohol consumption, so you may find that cutting down on the amount you drink improves your symptoms.
Management
The stomach does not sit in the middle of the body, it is on the left side with the opening therefore pointing up to the right. Therefore, laying on your left side may help to reduce the backflow of stomach contents, thus reducing your symptoms. If you prefer to sleep on your back, you may find that using more pillows can change the angle at which you lie, again reducing the backflow. If you are making changes with your pillows, ensure that your upper back is supported too, and you’re not just causing your neck to flex forward.
Beyond the lifestyle changes, your osteopath may be able to help by addressing the diaphragm. This is the large muscle within the rib cage that is responsible for efficient lung inflation. It also plays a role in supporting the sphincter at the top of the stomach. We assess the body as a whole when identifying problem areas, and we often find that alongside diaphragm dysfunction there will be tension in the upper back or elsewhere. Techniques and exercises may be appropriate for improving your reflux from a muscular perspective, and further treatment could help to limit secondary aches and pains from developing as a result.
Make an appointment to address reflux in Leeds here
References
- Singendonk, M., Goudswaard, E., Langendam, M., van Wijk, M., van Etten-Jamaludin, F., Benninga, M. and Tabbers, M., 2019. Prevalence of Gastroesophageal Reflux Disease Symptoms in Infants and Children: A Systematic Review. Journal of Pediatric Gastroenterology & Nutrition, 68(6), pp.811-817.
- Antunes C, Aleem A, Curtis SA. Gastroesophageal Reflux Disease. [Updated 2022 Jul 4]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK441938/
- Unicef.org. 2022. Feeding your baby: When to start with solid foods. [online] Available at: <https://www.unicef.org/parenting/food-nutrition/feeding-your-baby-when-to-start-solid-foods> [Accessed 8 August 2022].
- Lullabytrust.org.uk. 2022. The best sleeping position for your baby. [online] Available at: <https://www.lullabytrust.org.uk/safer-sleep-advice/sleeping-position/> [Accessed 8 August 2022].
- Holloway, R., 2000. The anti-reflux barrier and mechanisms of gastro-oesophageal reflux. Best Practice & Research Clinical Gastroenterology, 14(5), pp.681-699.