Early on in the pandemic, Long Covid emerged. It is now widely recognised as a potential complication of an infection with covid-19. This post-viral fatigue can last weeks or months after the initial infection, and although there is still a lot that has not been confirmed, we can now draw a few conclusions that may be beneficial for those seeking relief.
What is Long Covid (LC)?
The BMJ offered a definition in September 2020, before tests were readily available:
“not recovering [for] several weeks or months following the start of symptoms that were suggestive of covid, whether you were tested or not.” … [there is a] “distinction between very sick people who have recovered to an extent and [and have been] left with some impact of their severe sickness, versus those who had a relatively mild sickness from the start, in whom it is ongoing.”
So rather than LC being a case of covid that takes longer to overcome, it’s the persistence of some particular symptoms. Results from the Zoe app (published in October 2020) analysed the incidence of LC symptoms at 4, 8, and 12 weeks after the first symptoms. 13% still had symptoms at 4 weeks, 4.5% at 8 weeks, and 2% beyond 12 weeks.
Signs and Symptoms
A survey of people with LC identified the 50 most commonly reported symptoms. The top 10 were:
- Fatigue
- Muscle/body aches
- Shortness of breath
- Difficulty concentrating
- Inability to be active
- Headache
- Difficulty sleeping
- Anxiety
- Memory problems
- Dizziness
Nearly 1600 reported fatigue, but just over 1000 reported muscle aches, making fatigue the most widely reported symptom by far.
Joint and nerve pain were other commonly reported symptoms. Combined with the common symptoms of headache and muscle pains, it became apparent that patients may begin coming to osteopaths in search of relief. Interestingly, a lot of these symptoms overlap with fibromyalgia, namely the fatigue, body aches, cognitive issues, and poor sleep. Fibromyalgia is a condition that osteopaths may be able to help a patient manage.
There was a consideration that LC could be split into two sub-types: the respiratory based type characterised by most of the above symptoms, and a multi-system type. The multi-system type causes symptoms that affect brain, gut, and heart. Symptoms of difficulty concentrating or sleeping, anxiety, and memory problems could fall into this type.
Who is at Risk of Developing Long Covid?
LC seems to affect people who have had mild symptoms, rather than those who were hospitalised with the virus. As the vaccine programme rolled out, and fewer people developed a symptomatic illness, it seems that LC numbers have dropped.
Long Covid is also more likely to affect older people than younger. People with asthma are also at higher risk, as are people with a higher BMI.
One particularly interesting finding from the Zoe study was that:
the more symptoms a person had in the first week, the more likely they were to go on to develop long COVID.
This could mean an array of mild symptoms, even if their effect at the time is not particularly severe, could predispose someone to long covid more than someone who had one or two more major symptoms.
Identifying Long Covid
Diagnosis can be difficult, because LC is still quite a grey area. Lingering symptoms within 4 weeks of the initial infection may be somewhat expected, but beyond 28 days it may be considered LC. The top symptoms of LC can be quite vague, and you might find that you just feel “a bit off” rather than easily identifying the specific symptoms.
There is no test for LC, and antibody testing is unlikely to offer much information now that vaccines are widely available. At the time of writing, about 1/3 of the UK population has reported at least one positive lateral flow test in the UK. So it stands to reason that a significant proportion of the population would have antibodies, and only a fraction would have long covid.
Therefore, LC remains a clinical diagnosis based on history (and a recent positive test where possible).
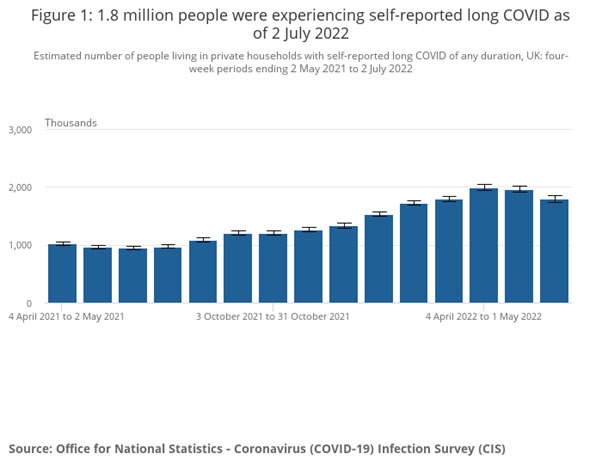
2022 Statistics
The ONS collected self-reported data in July 2022 to identify the extent of LC. An estimated 3% of the population was suffering from LC, of varying duration. 81% (1.4 million people) of those self-identifying with LC believed their first infection was from at least 12 weeks ago. 380, 000 believed their first infection was two years ago, although it is unclear whether their symptoms had been present since then, or from a subsequent infection.
This survey found the most commonly reported symptoms were:
- fatigue, affecting 54% of those reporting their LC
- shortness of breath, 31%
- loss of smell, 23%
- muscle aches, 22%
The ONS page continues to track the national estimate of LC cases over time. It is currently on a downward trajectory, with a peak occurring in April. At this point, an estimated 1.99 million people in the UK had long covid. This went down to 1.79 in June.
Potential Approaches
If you are suffering from a covid infection currently, do not underestimate the importance of rest and convalescence. Even if you’re fully vaccinated, you may find that the virus leaves you feeling exhausted or simply off-colour for quite a while, with lingering fatigue a definite possibility. Try not to overwork yourself while you still feel less than 100%, even if it takes a few weeks. General advice to make sure you eat well and stay hydrated through the length of your symptomatic period is sensible too.
The BMJ article mentioned above emphasised the importance of a multidisciplinary approach for patients with LC. This extends beyond the obvious respiratory and cardiovascular management, and monitoring for the expected improvements over time (safety netting). Another BMJ article broke down the elements of holistic healthcare that should be available for LC patients:
- Medical management (including investigations and specialist support where needed)
- Self management
- Social, financial, and cultural support
- Mental health support
- Management of comorbidities (such as diabetes, and heart or kidney problems)
Osteopathy and Self Management
Under the self management umbrella was “self pacing and gradual increase in exercise if tolerated“. It can be daunting knowing where to start; fortunately your osteopath can help you with this stage of rehabilitation. We can take into account what you are currently able to do, as well as what you used to do before LC and where you’d like to be eventually. Muscle mass is lost quickly, so don’t be too surprised if you feel weaker than you used to. This lost mass may impact the nuances in the way you move, so we will look closely at your current movements and make adjustments where needed to get you back on track. This might mean specific strengthening exercises to correct asymmetries, or more functional exercise to get the body moving as a unit again.
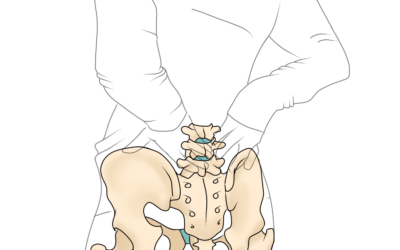
There may also be scope for osteopaths to help with the longer term musculoskeletal effects of disordered breathing and coughing. We know that when the diaphragm is working inefficiently, it recruits the accessory muscles of breathing around the shoulders and neck. These muscles do not cope well with extended use, as their role is just meant to be supportive. The same muscles can be overworked when breathing is difficult, or if you have a persistent cough. Secondary effects to fatigue of these muscles can include upper back stiffness, headaches, and lower back pain. We also know that some conditions are more likely to develop when local areas are working improperly, such as frozen shoulder. General osteopathic treatment after covid infection may help to prevent these problems.
Crossover with Fibromyalgia, CFS, or ME?
In addition to the comparisons made to fibromyalgia (above), there are also similarities with other conditions. Chronic fatigue syndrome (CFS) and myalgic encephalitis (ME) also cause symptoms of fatigue and more from the top 10 list. Although these conditions often seem to start for no apparent reason, we know that there sometimes seems to be a pattern of development after an infection. Although they are more than simple post-viral fatigue, there may be a similar mechanism at play for long covid.
ME patients who had covid also reported worsening of their usual ME symptoms. Given the similarities with these chronic pain conditions, there may be benefit in trying the techniques developed for those conditions. The Good Health Centre offers the Perrin Technique- a technique devised specifically for the treatment of ME and CFS. We’ve touched on the theory of using the Perrin Technique for Long Covid patients before.
Book here to address your Long Covid symptoms in Leeds
References
- Nabavi, N., 2020. Long covid: How to define it and how to manage it. BMJ, p.m3489.
- Health-study.joinzoe.com. 2020. One in 20 people likely to suffer from ‘Long COVID’, but who are they?. [online] Available at: <https://health-study.joinzoe.com/post/long-covid> [Accessed 22 June 2022].
- Shepherd, C., 2020. Covid 19 and Post Viral Fatigue Syndrome. [online] ME Association. Available at: <https://meassociation.org.uk/2020/04/covid-19-and-post-viral-fatigue-syndrome-by-dr-charles-shepherd-30-april-2020/> [Accessed 22 June 2022].
- Lambert, N., 2020. Results of Survivor Corps Long Hauler Survey July 25 2020. [online] Dig.abclocal.go.com. Available at: <https://dig.abclocal.go.com/wls/documents/2020/072720-wls-covid-symptom-study-doc.pdf> [Accessed 4 July 2022].
- Coronavirus.data.gov.uk. 2022. [online] Available at: <https://coronavirus.data.gov.uk/details/cases> [Accessed 8 August 2022].
- Ons.gov.uk. 2022. Prevalence of ongoing symptoms following coronavirus (COVID-19) infection in the UK – Office for National Statistics. [online] Available at: <https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/conditionsanddiseases/bulletins/prevalenceofongoingsymptomsfollowingcoronaviruscovid19infectionintheuk/4august2022> [Accessed 8 August 2022].
- Greenhalgh, T., Knight, M., A’Court, C., Buxton, M. and Husain, L., 2020. Management of post-acute covid-19 in primary care. BMJ, p.m3026.
- Shepherd, C., 2020. Covid-19 and Post-viral Fatigue Syndrome by Dr Charles Shepherd | 30 April 2020. [online] ME Association. Available at: <https://meassociation.org.uk/2020/04/covid-19-and-post-viral-fatigue-syndrome-by-dr-charles-shepherd-30-april-2020/> [Accessed 4 July 2022].
Comment *