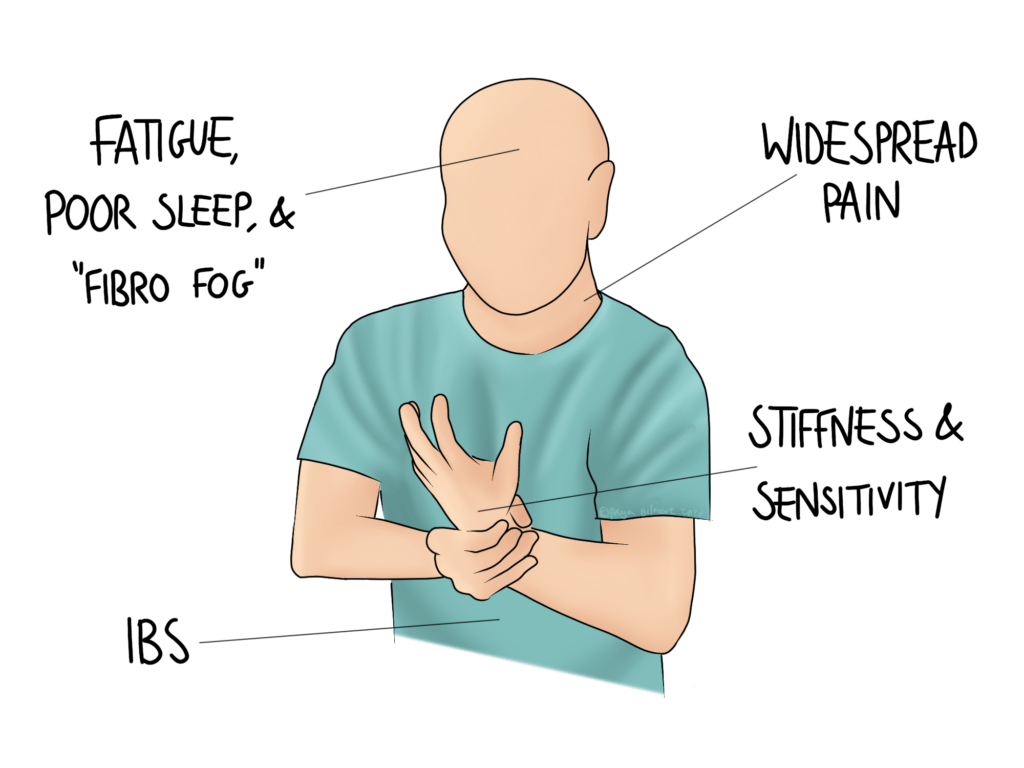
Symptoms of Fibromyalgia
Fibromyalgia is characterised by an array of symptoms lasting at least 3 months. These include:
- increased sensitivity to pain
- tender areas above and below the waist, on both the left and right sides of the body
- joint or muscle stiffness
- difficulty sleeping, and waking feeling unrefreshed
- extreme fatigue
- difficulty concentrating (and brain fog known as “fibro-fog”)
- headaches
- IBS symptoms (diarrhoea, cramps, constipation)
The severity is variable from person to person, but generally quite consistent for a single individual. It is diagnosed much more frequently in women than in men (only around 10% of patients are men), and symptoms tend to begin between the ages of 20 and 45. The onset can be quite mysterious, but for some people it follows some sort of trauma (including emotional trauma), or an infection. Symptoms of fibromyalgia have been reported in long covid studies, suggesting that covid-19 infection could be a trigger for some. This kind of onset is common to a few rheumatological conditions, some of which do share some symptoms with fibromyalgia, so investigation is important.
Diagnosis
There is no specific test for fibromyalgia, and it has a lot of similarities with a number of other conditions such as Rheumatoid Arthritis and inflammatory bowel disease (Crohn’s disease and Ulcerative Colitis). These should be ruled out in testing before a diagnosis is made. The criteria for diagnosis was updated in recent years. It focuses on the the widespread pain and other symptoms, with the requirement that symptoms have been present for 3 months or more. Importantly, there must be no other explanation for the pain (such as rheumatological conditions).
A questionnaire is used to rate the widespread pain and severity.
Widespread Pain Index (WPI)
This takes into account the areas in which you have experienced pain in the last seven days. There are 19 areas on the questionnaire, and each area scores a single point.
Symptom Severity (SS)
The symptom severity part of the questionnaire grades:
- fatigue
- waking unrefreshed
- cognitive symptoms (such as fibro-fog)
You will grade each symptom from a scale of 0 to 3:
0: no problem
1: slight or mild problems, generally mild or intermittent
2: moderate, considerable problems, often present and/or at a moderate level
3: severe: pervasive, continuous, life-disturbing problems
Finally, a score between 0-3 is given to reflect the general symptoms, which include things like hair loss, headaches, cramps, gastric symptoms, sensitivity to sun, and more.
A score is then calculated from this information. A score that could give a diagnosis of fibromyalgia is a WPI of 7 or more, with a SS of 5 or more. Alternatively, if SS was as high as 9, a WPI of 3-6 could also lead to a diagnosis.
Current Understanding of Fibromyalgia
Frustratingly, there is not a lot of certainty in the field. Even finding a specialist is difficult, as the condition is sometimes classified as rheumatological, and sometimes neurological. There is some overlap with Chronic Fatigue Syndrome and the controversial Trigger Points we discussed recently.
Potential Causes
Fibromyalgia is half classed as a Functional Neurological Disorder (FND), but it is also recognised to have more simple neurological hallmarks too. Most likely, the condition is caused by a mix of neurology, psychology, and potentially other pathologies too. A case study for the osteopathic treatment of fibromyalgia emphasised the importance of monitoring things like thyroid function as a part of the management strategy. A possible genetic link has been discussed too, which may explain patterns within families.
FNDs cover a broad range of symptoms, including things like blindness and seizures, but there is no evidence of a structural fault to explain them. IBS is an example of another functional condition. Often stress is a factor in the development of an FND, and this has been recognised within fibromyalgia too. None of this is to say that the symptoms are made up, as emphasised by the neurologist Suzanne O’Sullivan in her book It’s All In Your Head. She touches on her experiences with FNDs in this video:
Management Strategies for Fibromyalgia
Osteopathy is recognised as a therapy that may be able to help with management of fibromyalgia. However, progress is completely variable from person to person, and there is no recognised cure for fibromyalgia. A recent high quality study looking at a range of other published papers found little strong evidence for any one intervention. Even CBT and a couple of families of medications were only found to give a minor benefit. Interestingly, guidelines have ruled against the prescription of opioids for fibro.
The Perrin Technique
Some of our osteopaths have trained in the Perrin Technique to help people with Chronic Fatigue Syndrome (CFS) and ME. The similarities between these conditions and fibromyalgia means that we may also be able to use this technique to benefit our patients with fibro.
The technique follows a strict routine, focusing on a specific order of techniques to aid circulation of fluid within the body. Your first appointment will mostly entail discussion and case history taking, as well as a more detailed explanation of what you can expect. You are welcome to bring a chaperone if you would feel more comfortable to have a friend or relative with you. The techniques involve gentle motion through the limbs to aid the body’s natural pumping mechanisms in flushing through lymphatic fluid. There are also gentle massage techniques that aim to further move the lymph along. Ideas that fibromyalgia has some sort of association with general body inflammation could align with this treatment as a potential management strategy.
Therapeutic Exercise
Exercise is consistently shown to have some of the best outcomes for people with fibromyalgia. This contrasts strongly with patients who have ME, whose symptoms will be worsened by physical activity. Of course, when you’re fatigued and your muscles are sore, exercise does not appeal at all. Like any exercise, it’ll be easier if it’s something you enjoy, so we won’t work on getting you running if you detest it. If you have an exercise that you are interested to try, or used to enjoy, that would be a good place to start. Your osteopath can help you work out the correct dosage, although there is likely to be a bit of a trial and error involved.
There are a few things to consider about exercise now versus before your fibromyalgia.
- Overdoing it will likely cause your symptoms to flare.
- When gauging how you feel, pain is not the only consideration. PainScience.com recommends the Subjective Units of Distress Scale, which focuses on how you feel generally. Listen to your body and mind, and don’t feel that you need to push yourself too far.
- Take it day by day, and allow yourself more restful days when your symptoms are worse.
Beyond this, there is a lot of flexibility. Both cardio and strength exercise are considered beneficial, so let your preferences guide you there. Ideally, we will work with you to find a comfortable level of exercise (which will vary on good and bad days). From here, we can assess it in line with the progress you make generally, and increase the intensity, frequency, or duration of exercise as is comfortable.
As you return to exercise, you might find osteopathy to be particularly useful. We can treat minor sports injuries, but we also aim to prevent their development in the first place. If you feel that your form is not quite right, or that there are specific aches and pains associated with your exercise, let us know and we can look into it. Sometimes it’s as simple as one area of the body working a little less than it should, which can cause other areas to overload. Overloading is definitely something you would rather avoid if you are already sensitive to aches and pains, so nip them in the bud and let us know if there’s anything we can do to support your recovery.
Click here to make an appointment for your Fibromyalgia in Leeds
References
- Wolfe, F., Clauw, D., Fitzcharles, M., Goldenberg, D., Katz, R., Mease, P., Russell, A., Russell, I., Winfield, J. and Yunus, M., 2010. The American College of Rheumatology Preliminary Diagnostic Criteria for Fibromyalgia and Measurement of Symptom Severity. Arthritis Care & Research, 62(5), pp.600-610.
- Ingraham, P., 2022. [online] Available at: <https://www.painscience.com/articles/fibromyalgia.php> [Accessed 30 May 2022].
- Paul, L. and Berkowitz, M., 2015. Osteopathic manipulative treatment for an unusual presentation of fibromyalgia: A case report demonstrating the effectiveness of disease guidelines. International Journal of Osteopathic Medicine, 18(2), pp.141-147.
- Mayo Clinic. 2022. Fibromyalgia – Symptoms and causes. [online] Available at: <https://www.mayoclinic.org/diseases-conditions/fibromyalgia/symptoms-causes/syc-20354780> [Accessed 31 May 2022].
- Levi, M., 2020. Long covid and fibromyalgia or Chronic fatigue syndrome. [online] The BMJ. Available at: <https://www.bmj.com/content/370/bmj.m2815/rr-1> [Accessed 31 May 2022].
- Mascarenhas, R., Souza, M., Oliveira, M., Lacerda, A., Mendonça, V., Henschke, N. and Oliveira, V., 2021. Association of Therapies With Reduced Pain and Improved Quality of Life in Patients With Fibromyalgia. JAMA Internal Medicine, 181(1), p.104.
- Thieme, K., Mathys, M. and Turk, D., 2017. Evidenced-Based Guidelines on the Treatment of Fibromyalgia Patients: Are They Consistent and If Not, Why Not? Have Effective Psychological Treatments Been Overlooked?. The Journal of Pain, 18(7), pp.747-756.

0 Comments