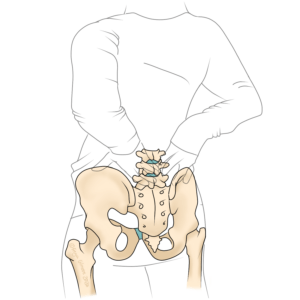
Lower back pain is one of the most common ailments that brings patients to clinic. Some people are prone to low grade, recurrent aches and pains. Others suffer from an acute episode that comes on for no apparent reason. Whatever the nature of your pain, we’re qualified to assess it. The vast majority of cases of lower back pain are considered “benign” (despite how they may feel!), and are within our remit for treatment.
Causes of Benign Lower Back Pain
- simple disc pain
- lower back pain associated with sciatica (without bladder or bowel changes)
- pulled or tight muscles
- ligament sprains within the back
- joint pain affecting the spine or back of the pelvis
- aches and pains associated with pregnancy
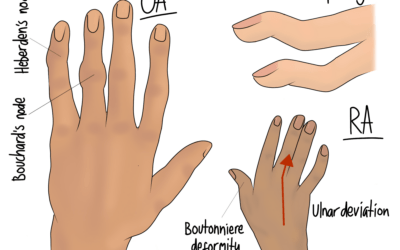
- arthritic pain
All of these causes will have some symptoms in common. But what you tell us in the initial case history will help us to prioritise a couple of diagnoses above the rest. Combined with the information we pick up from physical examination, we can give you a diagnosis before we start treating.
Arthritis in the Spine
Osteoarthritis is a common cause of joint pain, but people sometimes panic when they receive the diagnosis. One reason for this is that people often mistakenly believe that arthritis can only be managed with a joint replacement or injection. In fact, if symptoms are spotted early enough, improving your movement may be all you need to keep on top of the problem. This is particularly good news for people with spinal arthritis (spondylosis or spondyloarthrosis), because these joints cannot be easily replaced.
Things start to look a bit more optimistic when you understand that osteoarthritis is a condition of living tissue- primarily cartilage. Living tissue can heal from injury, albeit slowly in the case of cartilage. But there are things you can do to help it along, such as improving movement and encouraging the inflow of nutrients and removal of waste.
An osteopath can help you to regain movement in your back, and give you exercises to support this progress. We can also look elsewhere in the body for issues that might have overloaded the joint that has become arthritic.
Alongside movement, there are some other factors that play a role. Hydration, diet, and weight can influence the development and progression of arthritis. There are also factors, such as genetics, that are out of your control. Following current advice to maintain general good health is a good idea.
Sciatica with (or without) Lower Back Pain
Sciatica can be a common symptom associated with lower back pain. However, both sciatica and back pain can occur completely independently of one another.
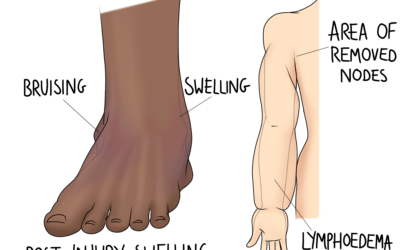
Sciatica describes a handful of symptoms caused by irritation of the sciatic nerve. This nerve runs from the lower back, through the pelvis, down the back of the thigh and down the calf. Symptoms can be felt anywhere from the back to the foot, and include typical nerve symptoms:
- pain, which is usually sharp or shooting
- a constant dull ache
- pins and needles or tingling
- numbness
- weakness
Some people also describe unusual sensations, like water running over their skin.
The above symptoms can also occur in the front of the leg. This might be due to a similar trapped nerve, but as long as it’s not the sciatic nerve, it’s not technically sciatica. On the other hand, not all pain in the leg is associated with a nerve. Issues in the lower back can cause pain to refer into the leg, or something unrelated like a hamstring injury can cause thigh pain.
Treating sciatica requires an understanding of the root cause. In some cases, a bulging disc or other structure in the back presses on the nerve to cause the symptoms. For other cases, there might just be a tight muscle in the buttock that’s causing the problem. Your osteopath will work on the root cause to resolve the problem. But we will also help with desensitising the nerve, especially in cases where the pain has been present for a long time. Giving a prognosis for sciatica is tricky, but generally the longer the pain has been there, the longer it will take to fully resolve. For this reason, we recommend seeking treatment as soon as you can for the best results.
If you have symptoms of sciatica in both legs, it may be a cause for concern. Read the information below on red flags if this might apply to you.
Discs Don’t Slip!
Pain is a complex thing, and your understanding of the issue makes a huge difference to the pain you feel. Patients often feel better before we’ve even touched them- just due to the reassurance of a professional telling them that it’s not as serious as they think. Disc injuries are quite misunderstood, with terms like “slipped disc” only making things worse. Worried patients might ask if we can feel the disc pushing out, but the reality is that the disc is very deep in the back, and only bulging: it’s not coming out of place.
The disc is a cylinder of cartilage with a soft centre. It helps with shock absorbance through the spine, and aids smooth movement. When demands are too great, the outer layer may be overstrained, and the middle might push against it. If this causes a bulge that pushes against a nerve, it can cause sciatica or other leg pain. Similarly, disc bulges that happen in the neck can cause arm pain. Discs don’t bulge forever: cartilage may be slow to heal but with appropriate movement, they do begin to knit back together.
Each disc is so firmly connected to the vertebra above and below, that the bones are more likely to break than the disc is likely to detach. Even in a condition called spondylolisthesis, where one vertebra slips forward on another due to fracture or unusual shaped bones, the disc still holds them together. So don’t worry that your discs are out of place. They are very firmly anchored, and your spine is stable.
Red Flags for Lower Back Pain
For the cases that are out of our remit, there are a handful of red flags that we look for. With this information, we can refer on to the most appropriate setting, whether that’s a non-urgent GP appointment or an ambulance to A&E.
Lower back pain that requires referral includes:
- suspected fractures
- infection
- rheumatological issues (although we may be able to help with symptoms after you receive a diagnosis and appropriate medication)
- pain following significant trauma
The NHS advises that you call 999 if your back pain is associated with any of the following:
- pain, tingling, weakness or numbness in both legs
- numbness or tingling around your genitals or buttocks
- difficulty peeing
- loss of bladder or bowel control (peeing or pooing yourself)
- chest pain
- it started after a serious accident, such as a car accident
The first few bullet points here apply to a rare but urgent condition called Cauda Equina Syndrome. The Cauda Equina (literally meaning “horse tail”) refers to the end of the spinal cord, where the nerves split within the spinal canal, resembling a horse’s tail. If these nerves are compressed, they can cause the symptoms listed above. The reason this is urgent is that without quick decompression, it can lead to permanent incontinence or paralysis. If your lower back pain is associated with changes to bladder and bowel habits, or numbness around the saddle area, go to A&E immediately.
Lower Back Pain During and After Pregnancy
Lower back pain is very common during pregnancy. The combination of hormonal changes and a shift in the centre of gravity puts a lot of strain on the back. Gentle treatment throughout pregnancy can help to redistribute forces in a more comfortable way. Muscle groups like the calves, hamstrings, and gluteal muscles are often overworked by the changing posture, and we can help with these too.
For expectant mothers suffering with more severe pain in the pelvis, we advise starting treatment as soon as possible. SPD: symphysis pubis dysfunction, causes pain and instability in the pelvis, and can affect your birthing options. Strengthening is recognised as a key part of a management plan for SPD. We can advise you here, and help to free up stiff areas elsewhere that may be putting extra strain on the pelvis.
We recommend that everyone has a Mummy MOT check up after birth, regardless of whether or not you have any symptoms. This comprehensive approach assesses the body as a whole, while at rest and moving, and involves an internal exam to check on the pelvic floor. If you suspect you have a pelvic organ prolapse, or are struggling with continence, this may be the treatment you need to get back to yourself. If you are 12 weeks or more post partum, you can book in through the link below. There’s no time limit on being postpartum, so even if your children have grown up and left home, we can still help with any pelvic floor or pelvic issues that developed in pregnancy.
Click here to make an appointment for your lower back pain in Leeds

0 Comments