Arthritic pain is an ailment that
osteopaths are qualified to help you to manage. Any joint can be affected, and there are a number of conditions that can cause the pain. It may manifest as a dull ache, or become sharp, and there may be associated symptoms elsewhere.
What is Arthritis?
Arthritis is a broad term referring to pain in a joint. Technically, the term alludes to inflammation specifically, but not all forms of arthritis are inflammatory. Of the types that are, there may still be pain between inflammatory episodes.
In the early stages, symptoms can be subtle. In some cases, the body responds before you feel a thing, for example, hip osteoarthritis can cause a change in the way you walk without the presence of any pain. As symptoms do develop, they can be subtle and hard to identify exactly.
Your osteopath can help you piece together the puzzle and begin treatment before the condition develops.
Red Flags and Arthritic Pain
If you don’t already have a diagnosis that would explain:
- redness over the affected joint
- skin that is warm to the touch
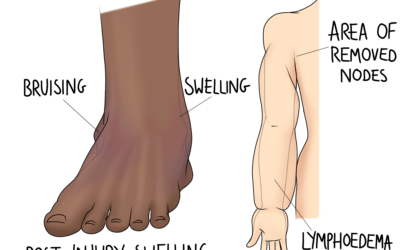
- local swelling
- or an increase in pain levels
Then you should seek help promptly. If you already have a diagnosis of an inflammatory arthritis, follow your doctor’s advice on when to investigate further, and how to manage flare ups.
If any of these symptoms present alongside a general feeling of unwellness, fever, or vomiting, seek medical attention urgently.
Osteoarthritic Pain
Osteoarthritis (OA) is a common cause of joint pain. It can affect any joint, often targeting the hips, knees, hands, and spine. The condition is considered “wear and tear” rather than a pathology as such, and it’s not all down to getting older. Injuries that have not been well rehabilitated, or recurrent injuries affecting the same joint can cause OA to develop sooner.
Osteoarthritis is a condition that affects the cartilage in a joint, and cartilage is living tissue. But it has a poor blood supply, and needs a flow of fluid around it to bring in nutrients and remove waste. While your range of movement is good, this works well. Using a joint through its full range allows the whole joint surface to be compressed and decompressed regularly, which squeezes out the waste and makes room for new fluid to flow in. The general movement in the joint also encourages new fluid to flow into the joint space.
But as movement becomes limited, such as following an injury or lifestyle changes, these processes become limited too. Less movement means some areas of cartilage are always compressed, and others are always decompressed. Neither area receives the new fluid or releases its waste. And general lack of movement allows old fluid to sit in the joint, holding more waste products than it should.
Our aim is to help you improve your every day movement through treatment and exercise. A hip with better range will then perform the “flushing out” movements described above to give the cartilage the best chance. In the early stages, this might be enough to keep the joint happy. But once the underlying bone becomes involved in the process (developing spurs or further injuries), the maximum amount of movement is limited further.
Joint Replacements due to Arthritic Pain
No one wants to undergo joint replacement surgery if it is avoidable. Fortunately, for osteoarthritis cases addressed early enough, the arthritic process can often be slowed, as described above. Looking after your joints by maintaining movement from the first sign of OA (or before) gives you the best chance of managing your symptoms conservatively. We can help you with a management strategy, providing exercises tailored for your affected joints. Some people find that group classes are more motivating than self-directed routines. Let us know if that resonates with you and we may be able to recommend a local class.
For cases where surgery is unavoidable, we still recommend
treatment for rehabilitation (and pre-habilitation, before surgery itself). These approaches help to prepare your body for the changes ahead, and adapt to them afterwards. We consider the effects on the rest of the body: gait changes that might cause an issue in the upper back, and local tissue changes for example.
Rheumatoid Arthritis
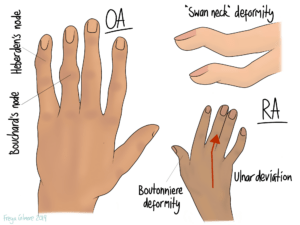
Rheumatoid arthritis (RA) is quite different to osteoarthritis, but the two are often confused. The pathological process of RA involves the body attacking a layer of the joint surface during inflammatory episodes. That makes it an autoimmune condition. Over time, the damage done, and the body’s attempted repairs, cause deformities in the affected joints. These are typically most obvious in the hands, where nodules form on the fingers, and the wrists turn outwards.
Besides the hands, the neck and feet are typically affected in the earlier stages. Larger joints may be affected later on. Pain tends to wax and wane in line with the condition’s inflammatory episodes. Symptoms are typically worse after rest, with longer lasting morning stiffness. Exercise helps to reduce symptoms, but too much activity will worsen them again. We expect symptoms to improve with anti inflammatory medications and in response to a cool compress. All of these features are slightly different to osteoarthritis, so if you’re unsure which kind of arthritis you have, we can give you a good idea from the case history alone. We may still want you to speak to your GP or seek a referral to rheumatology. This is because one important part of managing rheumatoid arthritis is medication. This can be taken alongside osteopathic treatment, but is a key strategy for minimising the frequency and extent of the flare ups.
Arthritic Pain in the Lower Back
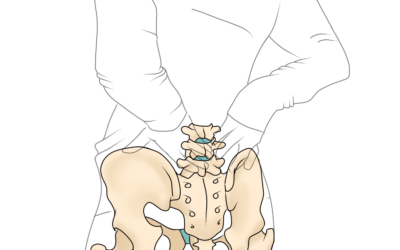
Although OA can be responsible for lower back pain, it is important that arthritic pain is as accurately diagnosed as possible. One other form of arthritis that causes back pain is
ankylosing spondylitis (AS). Unfortunately, this condition is often misdiagnosed as simple lower back pain for years. But like RA, there are medications that can modify the disease if taken early enough.
The name gives a good description of the process. Ankylosing means anchoring, and spondylitis means inflammation of the spine. Like with RA, AS has inflammatory episodes in which the joints at the base of the spine (and beyond) are attacked. The big issue is with healing- the body typically lays down new bone over the whole joint, causing stiffness over time. This new bone is fragile, and can be more vulnerable to fracture. This may just present as an increase in your usual back symptoms for a while, which again could just be brushed off as typical back pain.
There are some key symptoms that might point towards a diagnosis of AS. The part of the spine that is attacked is where tendons and ligaments attach to bone (the enthesis). Other areas in the body can be affected at the enthesis, most commonly where the Achilles tendon joins the heel bone. Because the condition is autoimmune, it has some connections to other conditions. A personal or family history of psoriasis or psoriatic arthritis, inflammatory bowel disease (Crohn’s or ulcerative colitis), or AS itself is significant. And if your pain is worse after rest but better with mild exercise, and responsive to ice rather than heat, there is a suggestion of an inflammatory pattern. Lower back pain combined with any of these symptoms may warrant further investigation.
Early diagnosis and intervention is key to a good outcome. The condition is relatively poorly understood, with some medical professionals unaware of the early signs. We can support you in your journey to a formal diagnosis, and we can continue to help you manage your pain afterwards. For good long term management, you need to know where your happy medium between rest and exercise lies. Meeting this sweet spot on a daily basis will help you to keep inflammation under control and therefore limit the damage done during an episode.
Managing Arthritic Pain
Your osteopath will develop a management plan based on your specific medical history, so everything is as appropriate and tailored as possible. The strategy may involve:
- further treatment to maintain mobility and reduce compensation elsewhere
- using heat or ice to relieve symptoms
- exercises to strengthen muscles or maintain joint health
- lifestyle changes, including dietary advice where appropriate, to better manage your flares.
Inflammatory arthritic pain is typically responsive to movement, but flares up again if movement is too intense or frequent. Finding your comfortable level and modality of exercise is key. We will also avoid over-treating, as it can have a similar effect to over-exercising.
If you have not yet had a formal diagnosis for your arthritis, this might be the first step we want to cover. We can support you with a referral back to the GP or onward to rheumatology where appropriate. Getting the correct medication might be the best chance available to minimise future flares and subsequent damage to the joints. With this under control, treatment can be more focused to residual symptomatic relief and addressing any compensatory patterns that have developed.

0 Comments