 This week is Arthritis Care Week in the UK. It aims to raise awareness of what it’s like to live with arthritis and is encouraging the 10 million people in the UK who have this degenerative condition to share their stories.
This week is Arthritis Care Week in the UK. It aims to raise awareness of what it’s like to live with arthritis and is encouraging the 10 million people in the UK who have this degenerative condition to share their stories.
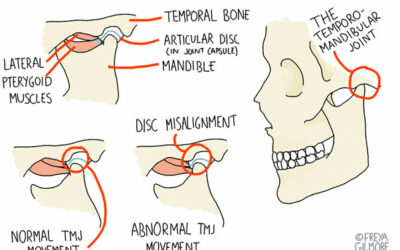
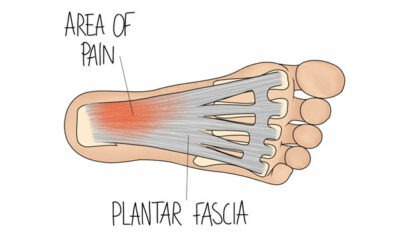
Arthritis is a common condition that causes pain, swelling, inflammation and often stiffness in joints of the body. The most common form or arthritis in the UK is osteoarthritis. Often referred to as ‘wear and tear’ on the joints of the body, it is a degenerative joint condition most common in the over 50s and affecting more women than men. Osteoarthritis most commonly affects the joints of the spine and neck, knees, hips and the base of the toes and hands.
We have written before about the complementary therapies that can bring relief from arthritic pain – click to read our post.
In this Arthritis Care Week post our osteopath Sebastian Contreras sets out in greater detail how osteopathy in particular can help people with arthritis to manage their condition. Seb says, “Just because you have been diagnosed with this degenerative condition, it doesn’t mean that nothing can be done to help prevent further deterioration, reduce your pain levels or improve your function.”
Seven ways osteopathy can help arthritis sufferers:
- Osteopathy treatment can mobilise the arthritic joint within a patient’s pain free ranges to maintain or increase their joint range of motion.
- Osteopaths can mobilise joints adjacent to the arthritic joint so that they can take some of the stress and strain off the pathological joint. For example, if a patient has an arthritic hip, we would commonly work on the joints in the low back to make sure they are working as well as possible.
- Treatments may also work on the adjacent muscles of the arthritic joint as these soft tissues can tighten up because of the altered function of the joint, causing pain. For example, in the case of an arthritic hip, the muscles of the groin can tighten.
- In some arthritis cases, patients are overweight. Being overweight puts more strain on the joints, which increases the chance of pain and further deterioration of the arthritic joint. But, because of the pain and stiffness associated with arthritis, it is often difficult to exercise to lose weight. Osteopaths can offer practical advice on how to lose weight with diet and exercise suitable for the individual patient.
- Certain foods have been shown to increase inflammation in the body, and therefore inflammation in the arthritic joint. These foods include processed sugar, fried food and red meat. By limiting, or better excluding, these foods from your diet, you can reduce the pain associated with inflammation in the arthritic joint.
- Our osteopaths can advise on certain strengthening of flexibility exercises that can help support or reduce pressure on the arthritic joint.
- Osteopaths can help with a maintenance programme. Since arthritis is an irreversible condition, osteopaths will encourage regular treatment – every 4 to 12 weeks once the acute phase of the pain has settled down. This is much the same as the way a dentist works, keeping on top of the body’s health before a bigger problem arises.
This month in the practice we’re recommending glucosamine complex capsules, particular for people with osteoarthritis. Glucosamine, which is found naturally in the body, plays an important role in making glycosaminoglycans and glycoproteins. These are essential building blocks of many parts of our joints, including ligaments, tendons, cartilage and synovial fluid. It’s been suggested that the way these parts of our joints are built and maintained contributes to the development and the progression of osteoarthritis.
If you or a loved one have arthritis and would like to learn more about how osteopathy may help you, get in touch with our reception team on 0113 237 1173 or click to request a call back.
0 Comments