The TMJ (temporomandibular joint) is the technical name for the jaw joint. TMD is a term sometimes used to mean “temporomandibular dysfunction”.
Problems Affecting the TMJ
The joint is unusual in its function and anatomy, and common problems affecting it include:
- pain
- locking
- clicking
- jerky or asymmetric movement
These symptoms may be consistent, or they might come and go. For variable symptoms, there may be a clear pattern to what causes your episodes, or it may seem to be completely random. People who suffer from TMD often don’t know which professional they should see, or they do not seek treatment for another reason.
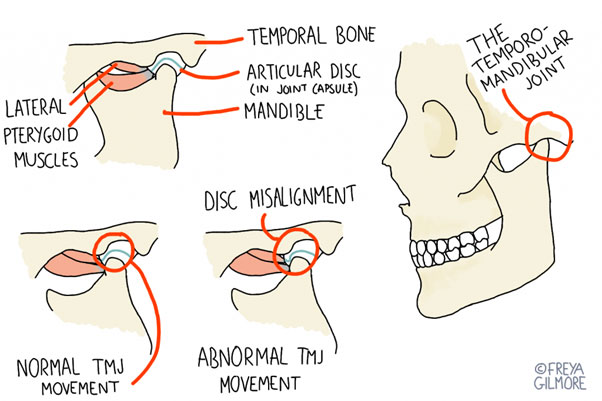
Anatomy of the TMJ
The jaw joint is mostly a hinge, but it also has the capacity to slide forwards when the mouth is open. The unusual movement is facilitated by a disc of cartilage within the joint, as well as the cartilage layer that covers the articulating bones. Another unusual point of anatomy is that one TMJ will directly influence the other, unlike the vast majority of joint pairs within the body. This does not mean that problems will always be symmetrical, but it might mean that your pain is more likely to affect both sides.
Arthritis in the Jaw
Osteoarthritis (OA) is the condition most commonly referred to simply as “arthritis”. Any joint with a cartilage component is capable of developing OA, and development of the condition can be slow and subtle. Early symptoms might include pain, which can be sharp or deep and dull. You might also notice a “grinding” quality to movement, whether that manifests as a resistance or a noise.
Some people hear a diagnosis of arthritis and assume it’s just something they have to tolerate until it progresses enough to warrant surgery. Fortunately, this is not always the case. If osteoarthritis is identified early, you can make changes to improve joint health and encourage the cartilage to heal. You can read more about osteoarthritis here.
Rheumatoid arthritis can affect the TMJ with similar symptoms to other problems. However, as it is rarely affects the TMJ in the early stages, it is more likely to present once a diagnosis of RA has already been made. Take note of any patterns to your jaw pain, are there any triggers that might be significant?
Disc Problems
The disc within the joint sits between the two bones within the joint, and allows smoother movement. But movement becomes jerky if the disc no longer slides smoothly over the surfaces. One potential cause for this involves tension in the cheek muscles. One of the deep muscles within the cheek attaches directly to the disc, and when under tension, can cause the disc to fold. This is particularly apparent when the mouth is wide open, as this is the movement that the muscles (as a pair) are responsible for.
You might experience this as a feeling of resistance when opening your mouth all the way. Alternatively, the jaw might move off to one side as you open it, before moving back into place at the end of the movement. Sometimes there is an audible click or crunch on these movements, or when biting down. Often it is this noise that causes patients to seek help, as it can be audible to other people as well as themselves. Fortunately, if the root cause of the problem is a tight muscle, treatment can be effective within a short period of time. However if the reason for the tightness is a longer term issue, such as bruxism (tooth grinding), it may take longer to fully resolve the issue.
Less frequently, we see patients whose TMD comes with locking when the jaw opens fully. This can be particularly embarrassing and stressful, often encouraging the patient to avoid opening their mouth all the way. We know that incomplete movements can change the demands on a joint and may predispose the development of osteoarthritis, so don’t suffer in silence.
We can give you exercises to help you unlock the jaw- sometimes it is the active effort to close it that blocks the movement further. Resisted exercises that encourage the jaw into a lateral movement, rather than trying to work straight through the restricted one, can help. These exercises can help for first aid, as well as having a longer term benefit to improve joint health and relax over-protective muscles.
Relationship with the Rest of the Body
Although the jaw is far from the centre of the body, it can still influence the structures around and below it. Likewise, adaptions made by the rest of the body can cause problems within the TMJ.
The diagram below shows the possible impact of a forward head posture on the jaw. You might develop this posture if you have sedentary demands on you, especially if you work at a desk with a screen that is maybe slightly too far away from you. If you move your head forwards, you might notice a slight pulling feeling in the front of the neck. It’s probably not significant enough to notice if you aren’t already drawing your attention to it. But it is significant. It demonstrates that the mechanical response to that forward shift of the head encourages the jaw to open.
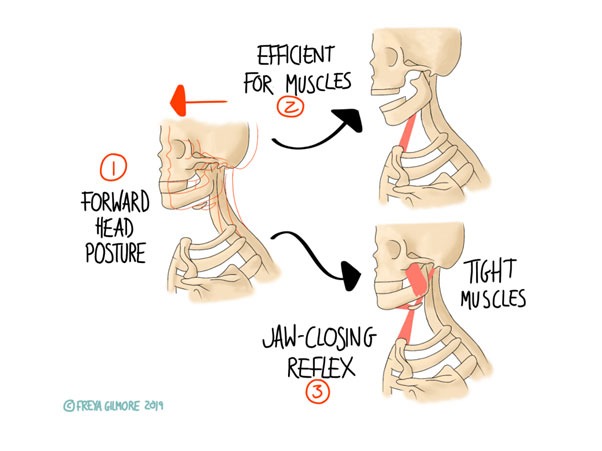
This puts tension on the muscles that close the jaw. Again, this may happen without you realising. This tension may result in teeth-grinding, which again may go unnoticed if it happens at night. Bruxism puts further pressure on the jaw joints and associated muscles. One possible complication of this is the development of trigger points. This can add another layer of uncertainty as trigger points within the jaw muscles can mimic pain further round the jaw and into the front of the face or the teeth. Treating the facial pain directly will likely be fruitless- we have to trace it back to the original cause.
Beyond effects on the jaw itself, that forward head posture puts higher demand on the muscles of the back of the neck, especially those at the base of the skull. Tension here can lead to headaches, which may only happen when you’re in that position, or they might be more persistent.
Osteopathic Management for the TMJ
Your osteopath is trained to look at the body as a whole to identify as many factors as possible in your presentation. If your TMD results from postural demands, we can work to identify why your posture is as it is. If it results from the demands of your desk, or your driving position, we can advise changes to make to improve this. Sometimes it comes from a discomfort or stiffness elsewhere, and it’s actually the compensation that’s causing the problem. In these cases, we may be working as far away from the TMJ as the back, pelvis, or even legs.
The body tries to keep the eyes and ears level, so asymmetry further down the spine may not correct until it reaches the neck, placing more asymmetric demands on the muscles around the neck and jaw. You may even find that your preventative strategy for TMD is centred on maintaining movement in the back to reduce demand on the head and neck.
For the TMJ itself, sometimes local work is exactly what you need. We have a range of techniques to hand, including direct or indirect, and internal or external techniques. We understand that work around the mouth and face can feel quite vulnerable, and we won’t do anything you’re uncomfortable with. Work for the muscles that affect the jaw can have surprisingly quick results, but as the problem rarely happens in isolation, it might return in the days or weeks following treatment. Exercises to maintain the progress, as well as an approach that addresses the other factors in the case, are key.
A Multidisciplinary Approach to the TMJ
For more complex presentations, work to improve head position and muscle tone may not be enough. One professional who can be particularly valuable for TMJ issues is your dentist. For people who grind their teeth, a guard or splint may be helpful. Whether it helps to break the cycle of bruxism or simply protects the teeth, it’s all a step in the right direction.
Malocclusion may also be a part of your TMD. If you have an underbite or overbite, the TMJ is the first joint affected. Of course malocclusion does not develop overnight, so your body may be well adapted to it. Alternatively, you might find that your bite places high demand on the joint and causes aches and pains. Sometimes these pains are clear from the outset. Other times it might only be apparent when arthritis develops years later.
Make an appointment for your TMJ in Leeds here
References
- Anuradha, A., Sodhi, A., Naik, S. and Pai, A., 2015. Rheumatoid arthritis affecting temporomandibular joint. Contemporary Clinical Dentistry, 6(1), p.124.
- Cuccia, A. and Caradonna, C., 2009. The Relationship Between the Stomatognathic System and Body Posture. Clinics, 64(1), pp.61-66.
- Andresen, T., Bahr, C. and Ciranna-Raab, C., 2013. Efficacy of osteopathy and other manual treatment approaches for malocclusion – A systematic review of evidence. International Journal of Osteopathic Medicine, 16(2), pp.99-113.
Please see Grace’s review video here :
Any questions please call 07718 115699
0 Comments