The name “plantar fasciitis” literally means “inflamed tissue on the sole of the foot”. However, the condition itself does not involve a significant amount of inflammation, and may be better classified as a somewhat degenerative condition rather than an inflammatory one.
Plantar Fasciitis Basics
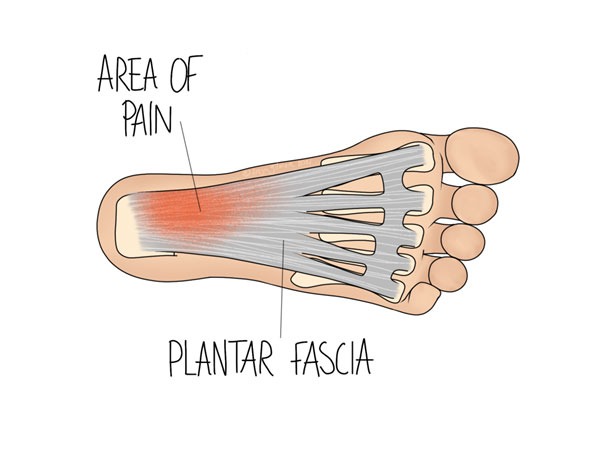
Fascia is a layer of tissue that sits between muscle and skin. There is a layer of fascia along the sole of the foot, and it blends with some other surrounding soft tissues. The illustration above shows the distribution of fascia in grey. This tissue’s job is primarily to maintain structure- it is not contractile like muscle tissue is, but it allows more movement than a ligament would.
Nothing in the body exists in isolation, and the plantar fascia is no exception. It has a close relationship with the muscles of the calf and the Achilles tendon. Tight calf muscles are noted as a risk factor in developing PF, and we often find in clinic that the calf does not function as well as possible in these cases.
Symptoms of Plantar Fasciitis
Plantar fasciitis (PF) typically begins with pain on the sole of the foot, just beyond the base of the heel. It is most often aggravated by stretching movements, such as going upstairs or wearing heeled shoes. We expect the average case to last at least 6 months, but less than a year.
Usually PF just affects one side, but about a third of cases affect both. We expect pain to be worse first thing in the morning or after a period of rest, such as sitting on the sofa for a while. You might also find that walking barefoot makes the pain worse, and that you may develop a limp or notice that you no longer touch your heel to the ground when walking. We recommend that you get started with treatment as soon as possible, but if you’ve started to develop new compensatory habits, see your osteopath as soon as you can to limit any secondary aches and pains.
Risk Factors
A number of issues with the way the foot mechanics work can predispose a person to developing PF. Therefore, it would be worth seeking osteopathic evaluation for any changes that you notice in your feet. Changes in arch height and altered heel mobility are key examples. Changes in the way you walk are important too, such as if you have to compensate for discomfort somewhere else. Other factors that might make someone susceptible to the condition include high BMI, diabetes, and problems with the muscles and soft tissues of the calf.
PF mostly affects people between the ages of 25 and 65, with an increase among over 40s. People who run regularly much more likely to develop it than the average person- roughly 10-20% of running related injuries are PF. One of the biggest factors that you have control over is how well your shoes fit: make sure you choose footwear that is supportive but not too tight or restrictive, avoiding very flat or high heeled shoes where possible.
Other Causes of Heel Pain
Although plantar fasciitis is common, affecting around 1/10 people at some point- it is not the only cause of pain in this area. Your osteopath will take a full case history, with focus on the details of onset and aggravating or relieving factors. This information may suggest another cause, which can be further tested on physical examination. Examples of conditions that may be mistaken for PF include:
- heel stress fracture
- arthritis
- local nerve irritation
- sciatica or other similar nerve irritation
- bursitis
- Achilles tendinopathy
Less commonly, the plantar fascia can rupture, causing some similar symptoms but with a few key differences. If your pain began very suddenly and there was bruising around the painful area, mention this to your osteopath so they can focus on the integrity of the tissue.
Management Strategies
NHS guidelines recommend exercises, and warn that injections are not always the best course of action. 90% of people respond well to gentle therapies such as osteopathy for PF. Stretches aim to relax the soft tissues on the sole of the foot, as well as the calf. You might find that stretching the foot against a wall or at the bottom of the stairs works well for you. Your osteopath can give customised advice for your exact situation.
Given the broad range of risk factors above, your osteopath will want to identify the root cause of your pain. We may find that there are areas within the foot that are over or underworking, so managing this balance might be appropriate for you. We can help to direct you to the right practitioner if it looks like orthotics or insoles might suit you too.
Click here to make an appointment for your foot pain in Leeds
References
- Physiopedia. 2022. Plantar Fasciitis. [online] Available at: <https://www.physio-pedia.com/Plantar_Fasciitis> [Accessed 13 June 2022].
- Cks.nice.org.uk. 2022. Scenario: Management | Management | Plantar fasciitis | CKS | NICE. [online] Available at: <https://cks.nice.org.uk/topics/plantar-fasciitis/management/management/> [Accessed 13 June 2022].
- Cks.nice.org.uk. 2022. Causes and risk factors | Background information | Plantar fasciitis | CKS | NICE. [online] Available at: <https://cks.nice.org.uk/topics/plantar-fasciitis/background-information/causes-risk-factors/> [Accessed 13 June 2022].
- Gill, L., 1997. Plantar Fasciitis: Diagnosis and Conservative Management. Journal of the American Academy of Orthopaedic Surgeons, 5(2), pp.109-117.
0 Comments