Trigger points are a controversial phenomenon as the research behind them is somewhat weak. What we know for certain is that they align with some people’s symptoms, so recognising them is still important. They seem to be more prevalent among people with conditions like fibromyalgia, who often feel somewhat invisible in a medical capacity.
Symptoms
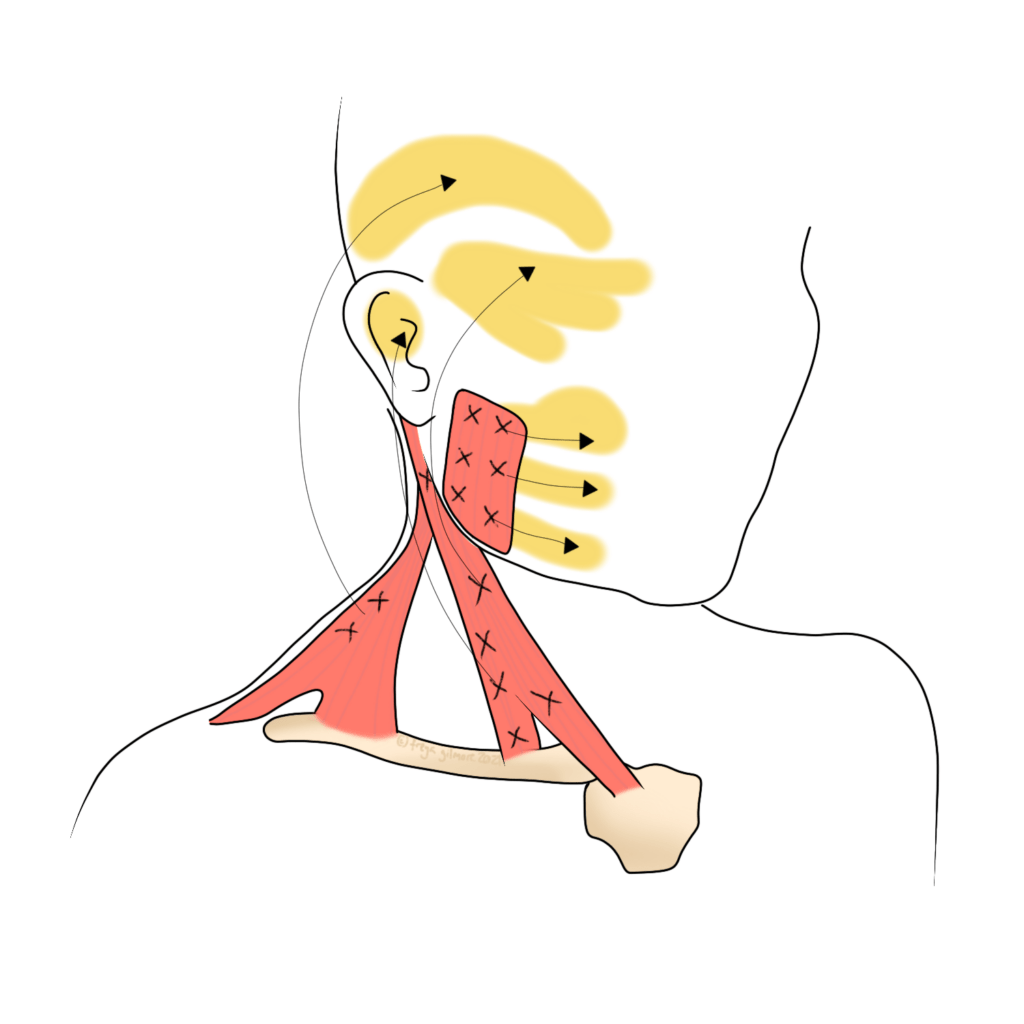
Trigger points can be very tender to touch, and cause a relatively predictable pattern of pain elsewhere. The illustration above shows some patterns of facial and head pain coming from trigger points in the neck.
Colloquially, they may be known as “knots”. This has been described as a “micro cramp”, and one theory is that this cramp is so severe that it affects those muscle fibres’ blood supply. Another theory is more concerned with the way the nerves and brain process the pain signals- the tissues themselves are relatively unremarkable.
Is it a Trigger Point or Sciatica?
Nerve pain, specifically radicular pain (the process behind sciatica), has some symptoms in common. Radicular pain is where a nerve is irritated, causing shooting pain, numbness, or weakness in the area the nerve supplies. Technically it is only called sciatica when it is the sciatic nerve that’s affected, but for simplicity, we’ll use sciatica as an example.
Both trigger points and sciatica cause pain in another area to where the real cause is. A trigger point in the buttock could cause pain down the thigh. Very similarly, a deep gluteal muscle (piriformis) can sometimes get tight and irritate the sciatic nerve, also causing pain down the thigh. A few features can differentiate between the two:
- the painful area in the leg will not be tender with a trigger point, but may be with sciatica
- the nature of the pain is achey, and vague in its distribution for the former. Sciatica is a more defined area of sharp, shooting or stabbing pain
Trigger Points vs Referred Pain
Referred pain is a much more widely accepted cousin of trigger points. Going back to sciatica again, referred pain from the back can often be mistaken for sciatica, but there are some important differences between the two. Although referred pain involved nerves, it is not the case that a nerve has been irritated by direct pressure, as is the case in sciatica. Symptoms are slightly different too- although referred pain from the lower back can cause pain in the same area as sciatica, it is not the same quality. Referred pain is much less likely to be sharp and shooting. Instead, it tends to cause a more dull or achey pain, which does not follow a defined line like sciatica.
The process behind referred pain is this:
- Something causes a signal to be sent to the brain to alert it of pain or danger
- The signal is sent along the nerve that supplies the affected area
- For some reason, the brain misinterprets the exact point the signal is coming from, and instead thinks it’s coming from somewhere else in the signalling nerve’s remit
- Therefore the pain is felt in the wrong place
Fortunately, we are all wired similarly. If you have symptoms of referred pain, we can map out the area that it is most likely coming from: the area supplied by the affected nerve.
Managing Trigger Points
As the science behind them is murky, the perfect treatment for any individual can be tricky to pin down. Sometimes, the solution is as simple as finally treating the trigger point, rather than the area where symptoms are felt. Following the theory that a trigger point is just a hyper-contracted group of muscle fibres, it would make sense that massage type techniques could help. Contrary to popular belief, massage is not about physically “breaking up” knots. Instead, it works by sending a message to the brain to relax the muscle. If treatment involves the nervous system, maybe this would help if the other theory is right, and trigger points are an issue of neurology.
Alongside direct treatment to the affected muscle, we may also look further afield in your treatment. Our aim here is to find other areas that are either affected by the trigger point, or to find those that may have had a role in developing it. Treatment to improve mobility in nearby joints may be helpful, and we can provide exercises especially for your case to help you maintain (or further improve) your progress between appointments.
Of course, trigger points would not be such a hot topic if they always responded like other tight muscles. We have a range of therapies available at the Good Health Centre that may help, including Osteopathy and Acupuncture. You can make an appointment using the link below, or contact us if you’d like to discuss which therapy might be most appropriate for you specifically.
Click here to make an appointment for your pain in Leeds
References
- Lempp, H., Hatch, S., Carville, S. and Choy, E., 2009. Patients’ experiences of living with and receiving treatment for fibromyalgia syndrome: a qualitative study. BMC Musculoskeletal Disorders, 10(1).
- Ingraham, P., 2022. The Complete Guide to Trigger Points & Myofascial Pain. [online] PainScience. Available at: <https://www.painscience.com/tutorials/trigger-points.php> [Accessed 5 May 2022].
- Alvarez, D. and Rockwell, P., 2002. Trigger Points: Diagnosis and Management. Am Fam Physician, 65(4), pp.653-661.